Introduction
Osteogenesis imperfecta (OI) is a heterogeneous genetic syndrome of the connective tissue that is caused by a defect in the gene that produces type I collagen, a protein found mainly in the bones and skin and synthesized in the endoplasmic reticulum in the form of precursor molecules pro-alpha1 and pro-alpha2 chains. Defects in the structure and amount of collagen, in the intracellular transport of this protein, as well as in its incorporation into the bone matrix are observed in patients with OI. Since type I collagen provides tissue support and tensile strength, OI causes bone fragility, increasing the risk of multiple fractures and subsequent limb deformities.1
In 1979, Sillence et al.2 classified OI into four clinical types based on the phenotypic presentation of the disease. However, in the following decades, the discovery of de novo mutations led to an increase in the number of OI types, and modifications to the Sillence et al.2 classification have been proposed, such as the addition of 3 types proposed by Rauch and Glorieux in 1998.3 Likewise, in the last decade, several genetic mutations have been discovered, resulting in OI being classified into 18 types.4,5
The clinical presentation of OI is varied and depends on the severity of the type. These patients may present with hearing loss or deafness, cardiovascular disease, and psychological, dental and endocrine disorders. Less severe types of OI are diagnosed clinically, and their characteristic signs include blue sclera, frequent fractures, long bone deformity, short stature, among others. Lethal types of OI, such as OI type II (perinatal lethal), are usually diagnosed during gestation.5 A genetic study is also recommended in order to determine the mutation of the gene that caused the disease.
Bone deformities observed in children with this disorder vary depending on the OI type and, in this sense, the most severe deformities are observed in children with type III OI.1 Moreover, in these patients, fractures occur more frequently in long bones such as the femur, tibia, and humerus. It has also been reported that OI treatment with bisphosphonates since its diagnosis reduces the frequency of fractures as a complication of this condition. However, the management of fractures depends on the patient’s age, the type of fracture, the fractured bone, the bone segment involved, the loadbearing capacity, and the risk of refracture.
OI causes spinal deformities, so its manifestations include scoliosis or kyphosis; thoracic deformity and decreased pulmonary function; craniocervical junction abnormalities such as basilar impression, basilar invagination, platybasia, and even nerve compression; and spondylolisthesis in the lumbosacral region.5
On the other hand, coxa vara is a femoral neck deformity defined as a neck-shaft angle >110° and can occur in up to 10% of patients with OI, most frequently in those with type III OI and, less frequently, in those with type I OI. Clinical manifestations of coxa vara include gait disturbance, leg shortening, Trendelenburg gait, genu valgum, and pain. Regarding imaging studies, an x-ray of the pelvis and the entire lower extremity with axial or lateral projection is necessary in order to corroborate the diagnosis of coxa vara, since a false image of coxa vara can be observed in antero-posterior pelvis x-ray imaging due to the presence of an anterior deformity of the femur, which is common in children with OI.1,6
Indications for surgical treatment of coxa vara are hilgenreiner-epiphyseal angle (HEA) ˃60° or neck-shaft angle (CDA) ˂110°, documented progression of varus deformity, and gait disturbance (limping).1 The objectives of this surgery are to correct the deformity to avoid fractures and progression of genu varum, to improve the weight-bearing line (which will allow the patient to walk without difficulty), and to restore abductor leverage in order to promote proper acetabular development. Considering the foregoing, the aim of this article is to present the results of the use of a surgical technique in the treatment of coxa vara in two children with OI.
Case presentation
Boys aged 13 and 8 years with a diagnosis of type III OI, with positive Trendelenburg sign, adequate joint mobility, and a history of recurrent fractures and previous surgeries for deformities, who underwent surgery for coxa vara correction at the Hospital Pediátrico Baca Ortiz (Quito, Ecuador). It should also be noted that both patients presented reduction of the left lower limb (4 and 2 cm, respectively), and the 8-year-old patient needed support for ambulation. Radiographic and functional evaluation (Harris scale) was performed 6 and 68 months after surgery, respectively.
The surgical technique used in both surgeries and the results in each case are described below.
Surgical technique
The surgical technique used in both patients was described in 2008 by Fassier et al.7 Under general anesthesia, the patient is placed in the supine position on the x-ray transparent operating table. Then, a standard posterolateral approach to the femur extended to the greater trochanter is made and, with fluoroscopic guidance, two smooth K-wires are placed along the femoral neck in a triangle position towards the femoral head to allow insertion of the telescopic nail (Figure 1A). Subsequently, using an image intensifier, the osteotomy site is established (Figure 1B) b) and the 2 Kirschner wires are used as a joystick, allowing safe adduction of the proximal femoral fragment without the need to use a bone holding forceps (Figure 1C). At this point, with a drill bit, whose size varies depending on the diameter of the wire to be inserted (e.g., in the cases reported here a 4.5 mm drill bit was used), a hole is drilled in the side cortex of the proximal femoral metaphysis, and then the drill bit is pushed through the superior cortex of the adducted fragment (Figure 1D).
The medial cortex of the distal femoral segment is then removed (Figure 1E). Next, the telescopic intramedullary nail is inserted from the greater trochanter and slid down to the distal shaft (Figure 1F). Finally, the K-wires are bent and secured to the shaft with cerclage wire (Figure 1G).
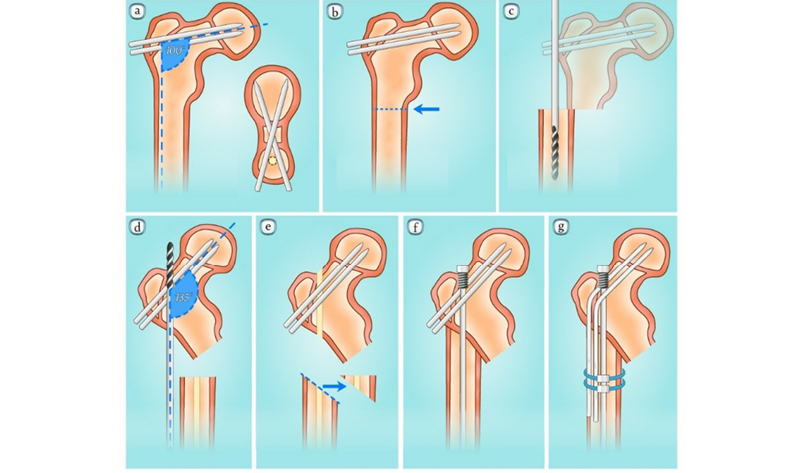
Figure 1. Surgical technique steps used in coxa vara correction surgery.
Source: Adapted from Hamdy.1
Results
In case 1, the neck-shaft angle was corrected by 46° during surgery (initial angle: 84°; final angle: 130°) (Figure 2). At 68-month follow-up, the Harris scale score was 70. Finally, regarding the reduction of the lower limb (initially 4 cm), a correction of 3 cm was observed.
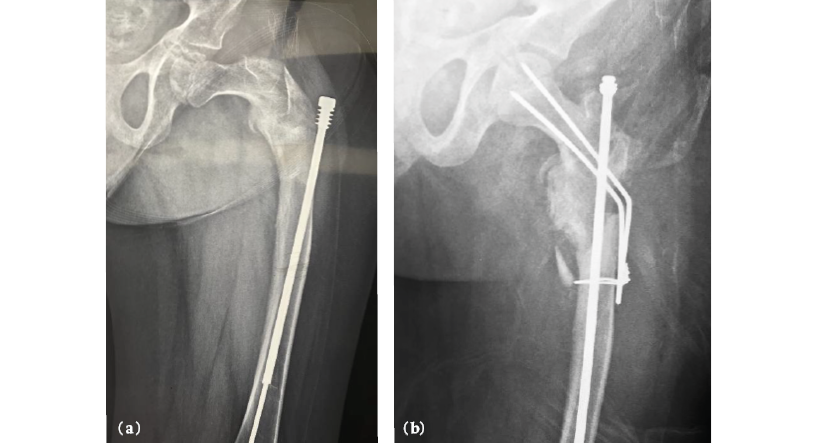
Figure 2. Case 1. A) Anterior-posterior x-ray of the left hip showing a neck-shaft angle of 84° (before surgery). B) Anterior-posterior x-ray of the left hip showing a neck-shaft angle of 130° (after surgery).
Source: Images obtained during the study.
In case 2, the neck-shaft angle was corrected by 50° with surgery (initial angle: 82°; final angle: 132°) (Figure 3). At the 68-month follow-up, the patient obtained a score of 68 on the Harris scale. Finally, regarding the reduction of the lower limb (initially 2 cm), a correction of 1 cm was observed.
b)
)
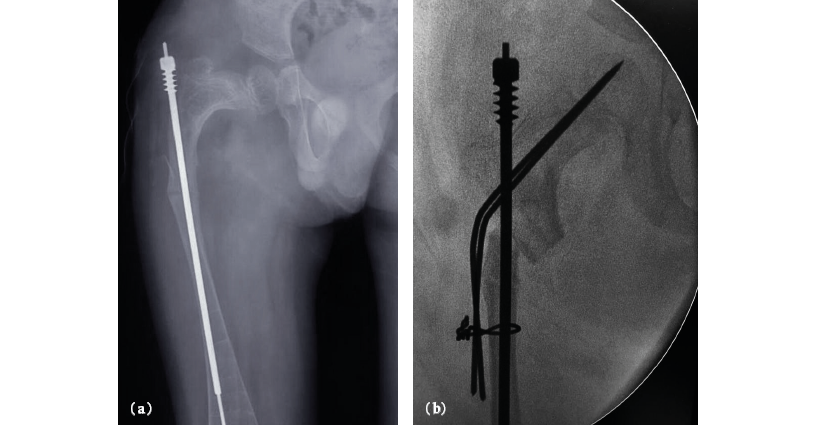
Figure 3. Case 2. Anterior-posterior x-ray of the right hip, showing a neck-shaft angle of 82° (before surgery). B) Anterior-posterior x-ray of the right hip, showing a neck-shaft angle of 132° (after surgery).
Source: Images obtained during the study.
The main characteristics of each case and the results (radiological and functional) obtained with surgery are presented in Table 1.
Table 1. Main characteristics of patients and radiological and functional findings.
|
Identification |
Age |
Type of osteogenesis imperfecta |
Initial neck-shaft angle |
Neck-shaft angle after surgery |
Initial HEA angle |
HEA angle after surgery |
Initial range of motion |
Range of motion after surgery (6 months) |
Initial score on Harris scale |
Harris score after surgery |
|
Caso 1 |
13 years old |
Type III |
84° |
130° |
76° |
30° |
Flexion: 90° Extension: -5° External rotation: 15° Internal rotation: 20° |
Flexion: 95° Extension: 5° External rotation: 20° Internal rotation: 20° |
56 |
70 |
|
Caso 2 |
8 years old |
Type III |
82° |
132° |
75° |
28° |
Flexion: 90° Extension: 0° External rotation: 20° Internal rotation: 20° |
Flexion: 95° Extension: 5° External rotation: 20° Internal rotation: 20° |
48 |
68 |
HEA: Hilgenreiner-epiphyseal angle.
Source: Own elaboration.
Discussion
One of the first techniques to correct coxa vara in patients with bone diseases, such as OI and fibrous dysplasia, was described by Wagner, in which a subtrochanteric osteotomy fixed with K-wires and its cerclage to the femoral diaphysis is performed. In 1988, Finidori developed a variation on Wagner’s technique, using telescopic nails to maintain and improve osteotomy consolidation. Later, in 2003, Fassier combined both techniques using the Fassier-Duval telescopic nail and modified aspects such as the necessary reaming for nail placement, perforating the lateral femoral cortex to allow passage of the nail when performing the genu varum correction maneuver, and excising a fragment of the medial cortex of the distal femur.8,9
On the other hand, according to Burnei et al.,10 the insertion point of the telescopic nail can correct both genu varum and genu valgum deformities. Moreover, the importance of preoperative planning in these cases has been pointed out, which consists of determining the desired neck-shaft angle on an x-ray and defining the insertion point of the endomedullary nail preoperatively.11
An additional variation of the technique used by Frasser in 2003 was performed by Logheswaren et al.12 in two cases of proximal femur deformity in pediatric patients with OI and fibrous dysplasia. This technique involved a subtrochanteric osteotomy and the use of a Rush pin and K-wires. The surgery results were satisfactory since the limb was lengthened and mobility for ambulation was maintained.
In a study published in 2019, Srisaarn et al.13 evaluated 31 patients (34 hips) aged 5 to 30 years who underwent coxa vara correction surgery between 2005 and 2014. In adolescent patients, they used the technique described by Finidori and placed plate and nail, while in adults, they used gamma nail plus dynamic compression plates or angle blade plate. In their study, the results of the procedure were satisfactory, the deformity was corrected, achieving a neck-shaft angle of 120°-135° and an average score of 79.68 on the Harris scale.
Conclusions
The objective of the subtrochanteric osteotomy surgical technique with endomedullary nails and Kirchner wires is the correction of the neck-shaft angle. Although several techniques have been described for its correction, high recurrence rates (30-70%) have been reported. Due to the underlying bone disease in the children described in this report, there is a high risk of mechanical loosening of the implants used in osteotomies, such as the plate and screws. However, by using these two types of nails, the technique reduces the risk of mechanical failure and provides stability to the osteotomy. Furthermore, in the two described cases, adequate neck-shaft angle correction was achieved, and good mobility and Harris scale scores of 68 and 70 points were attained.
In children with decreased bone density or diseases that alter collagen production, the objective of this surgery is to improve the patients’ quality of life by correcting the anatomy of the hip.
Based on our experience, the correction technique using endomedullary nails and K-wires is an effective option for the treatment of coxa vara in patients with OI. However, it should be noted that this technique requires an extensive learning curve from the orthopedic surgeon due to the associated transoperative and postoperative complications. Finally, it should be pointed out that one of its main advantages is the correction of the large amplitude of the neck-shaft angle.
Ethical considerations
Informed consent was obtained from the legal guardians of both patients for the preparation of this case report.
References
1.Hamdy RC. Coxa Vara in Osteogenesis Imperfecta. En Hamdy RC, Saran N, editores. Pediatric Pelvic and Proximal Femoral Osteotomies. A Case Based-Approach. Springler Cham; 2018. 223-33. https://doi.org/j2x5.
2.Sillence D, Senn A, Danks DM. Genetic heterogeneity in osteogenesis imperfecta. J Med Genet. 1979;16(2):1101-16. https://doi.org/fbqnqn.
3.Rauch F, Glorieux FH. Osteogenesis imperfecta. Lancet. 2004;363(9418):1377-85. https://doi.org/fg5kq6.
4.Van Dijk E, Sillence D. Osteogenesis Imperfecta: Clinical Diagnosis, Nomenclature and Severity Assessment. Am J Med Genet Part A. 2014;164A(6):1470-81. https://doi.org/f54prg.
5.Franzone J, Shah S, Wallace M, Kruse, RW. Osteogenesis Imperfecta A Pediatric Orthopedic Perspective. Orthop Clin North Am. 2019;50(2):193–209.
6.Aarabi M, Rauch F, Hamdy RC, Frassier F. High prevalence of coxa vara in patients with severe osteogenesis imperfecta. J Pediatr Orthop. 2006; 26(1):24–8.
7.Fassier F, Sardar Z, Aarabi M, Odent T, Haque T, Hamdy R. Results and Complications of a Surgical Technique for Correction of Coxa Vara in Children With Osteopenic Bones. J Pediatr Orthop. 2008;28(8):799-805. https://doi.org/b294n8.
8.Finidori G. Ostéogènese imparfaite. Indications thérapeutiques chez l’ enfant. Paris: Conférences d’ensegnement. Cahier d ́enseignement de la SOFCOT; 1988.
9.Finidori G, Topouchian V. Ostéosynthèses centro-médullaires palliatives chez l’enfant atteint d’ostéogenèse imparfait [Internet]. 2016. [cited Nov 2019] Available from: https://www.medicalex.info/wp-content/uploads/docteur_Finidori.pdf.
10.Burnei G, Vlad C, Georgescu I, Gavriliu T, Dan D. Osteogenesis Imperfecta: Diagnosis and Treatment. J Am Acad Orthop Surg. 2008;16(6):356–66. https://doi.org/f3vzgh.
11.Scollan JP, Jauregui JJ, Jacobsen CM, Abzug JM. The Outcomes of Nonelongating Intramedullary Fixation of the Lower Extremity for Pediatric Osteogenesis Imperfecta Patients: A Meta-analysis. J Pediatr Orthop. 2017;37(5):e313-6. https://doi.org/gbkmpf.
12.Logheswaren S, Sulaiman AR, Munajat I. A Modified Technique of Fixation for Proximal Femoral Valgus Osteotomy in Abnormal Bone: A Report of Two Cases. Malaysian Orthop J. 2017;11(2):82-4. https://doi.org/j25c.
13.Srisaarn T, Salang K, Klawson B, Vipulakorn K, Chalayon O, Eamsobhana P. Surgical correction of coxa vara: Evaluation of neck shaft angle, Hilgenreiner-epiphyseal angle for indication of recurrence. J Clin Orthop Trauma. 2019;10(3):593-8. https://doi.org/j25d.